The concept sounds like the stuff of science fiction: take a pill, and suddenly new tissues grow to replace damaged ones
Researchers at Case Western Reserve and UT Southwestern Medical Center this week announced that they have taken significant steps toward turning this once-improbable idea into a vivid reality. In a study published in the June 12 edition of Science, they detail how a new drug repaired damage to the colon, liver and bone marrow in animal models — even going so far as to save the lives of mice who otherwise would have died in a bone marrow transplantation model.
“We are very excited,” said Sanford Markowitz, MD, PhD, the Ingalls Professor of Cancer Genetics at the university’s School of Medicine and a medical oncologist at University Hospitals Case Medical Center’s Seidman Cancer Center. “We have developed a drug that acts like a vitamin for tissue stem cells, stimulating their ability to repair tissues more quickly. The drug heals damage in multiple tissues, which suggests to us that it may have applications in treating many diseases.”
The institutions collaborating on this work next hope to develop the drug — now known as “SW033291” — for use in human patients. Because of the areas of initial success, they first would focus on individuals who are receiving bone marrow transplants, individuals with ulcerative colitis, and individuals having liver surgery. The goal for each is the same: to increase dramatically the chances of a more rapid and successful recovery.
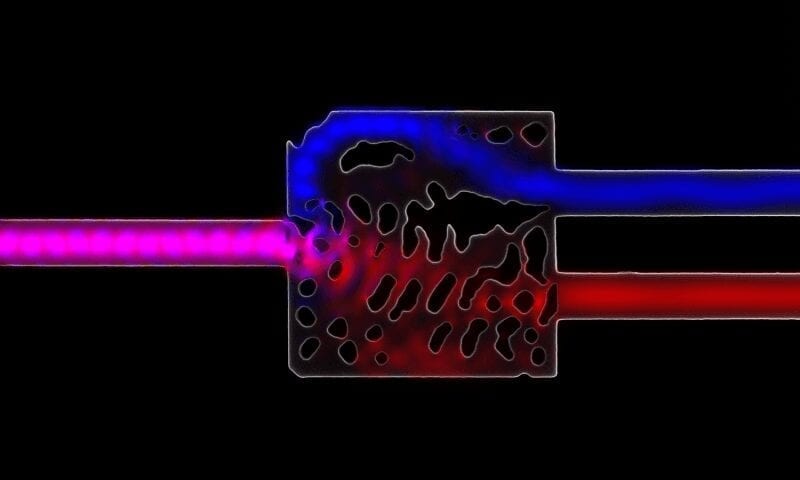
The key to the drug’s potential involves a molecule the body produces that is known as prostaglandin E2, or PGE2. It is well established that PGE2 supports proliferation of many types of tissue stem cells. Markowitz and University of Kentucky Professor Hsin-Hsiung Tai earlier had demonstrated that a gene product found in all humans, 15-hydroxyprostaglandin dehydrogenase (15-PGDH), degrades and reduces the amount of PGE2 in the body.
Markowitz, also a Harrington Discovery Institute Scholar-Innovator, and James K.V. Willson, MD, a former Case Western Reserve colleague now at UT-Southwestern, hypothesized that inhibiting 15-PGDH would increase PGE2 in tissues. In so doing, it would promote and speed tissue healing. When experiments on mice genetically engineered to lack 15-PGDH proved them correct, the pair began searching for a way to inactivate 15-PGDH on a short-term basis.
The preliminary work began in test tubes. Yongyou Zhang, PhD, a Case Western Reserve research associate in Markowitz’s lab and a lead author on the study, developed a test where cells glowed when 15-PGDH levels changed. Zhang then traveled to UT Southwestern’s Harold C. Simmons Comprehensive Cancer Center, where Willson serves as director. Zhang and UT Southwestern researchers Bruce Posner, PhD, and Joseph Ready, PhD, collaborated to comb through the center’s library of 230,000 different chemicals. Ultimately they identified one chemical that they found inactivated 15-PGDH.
“The chemical, SW033291, acts in an incredibly potent way,” Markowitz said. “It can inactivate 15-PGDH when added at one part in 10 billion into a reaction mixture, which means it has promise to work as a drug.”
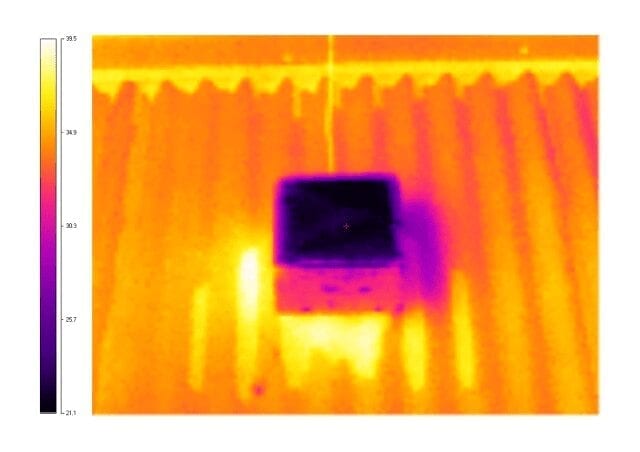
A series of experiments showed that SW033291 could inactivate 15-PGDH in a test tube and inside a cell, and, most importantly, when injected into animal models. The third finding came through collaboration between Markowitz and Stanton L. Gerson, MD, director of the Case Comprehensive Cancer Center, UH Seidman Cancer Center, and the National Center for Regenerative Medicine, as well as the Asa and Patricia Shiverick-Jane Shiverick (Tripp) Professor of Hematological Oncology.
Case Western Reserve research associate Amar Desai, PhD, worked between the Markowitz and Gerson laboratories to determine the effect of SW033291 on mice that had received lethal doses of radiation and then received a partial bone marrow transplant. Without SW033291, the animals died. With it, they recovered.
From there, more detailed studies showed that mice given SW033291 recovered normal blood counts six days faster than mice that were transplanted without receiving SW033291. In addition, SW033291-treated mice showed faster recovery of neutrophils, platelets and red blood cells. Neutrophils battle infection, platelets prevent bleeding, and red blood cells deliver oxygen throughout the body.
In addition, Desai’s work showed that when SW033291 increases PGE2 in bone marrow, the body also begins to produce other materials that bone marrow stem cells need to survive. Finally, these benefits emerged without any adverse side effects, even at SW033291 doses much higher than would be required for 15-PGDH inhibition.
When investigators treated mice with other diseases, the SW033291 drug again accelerated tissue recovery. For example, the investigators teamed with Fabio Cominelli, MD, PhD, a Case Western Reserve Professor and Chief of the Division of Gastroenterology and Liver Disease, to study a mouse model of ulcerative colitis. SW033291 healed virtually all the ulcers in the animals’ colons and prevented colitis symptoms. In mice where two-thirds of their livers had been removed surgically, SW033291 accelerated regrowth of new liver nearly twice as fast as normally happens without medication.
Read more: New drug triggers tissue regeneration: Faster regrowth and healing of damaged tissues
The Latest on: Tissue regeneration
[google_news title=”” keyword=”Tissue regeneration” num_posts=”10″ blurb_length=”0″ show_thumb=”left”]
via Google News
The Latest on: Tissue regeneration
- Novel fabrication method creates aligned nanofiber hydrogels for tissue regenerationon May 3, 2024 at 10:12 pm
A team of chemists and bioengineers at Rice University and the University of Houston have achieved a significant milestone in their work to create a biomaterial that can be used to grow biological ...
- Scientists uncover a cell responsible for repairing damaged liver tissueon May 2, 2024 at 10:48 pm
A type of cell responsible for repairing damaged liver tissue has been uncovered for the first time by a team of scientists, including Professor Rajiv Jalan (UCL Liver & Digestive Health).
- Study pinpoints cell that helps liver healon May 2, 2024 at 6:22 am
A type of cell responsible for repairing damaged liver tissue has been uncovered for the first time by scientists.
- Study: Hillocks challenge our understanding of lung biologyon May 1, 2024 at 9:28 am
Airway hillocks are mysterious, flat-topped structures that were only recently identified within regular lung tissue, and their role in airway ...
- Kerecis to Provide Multiple Updates on its Medical-Fish-Skin Technology at the European Wound Management Association Meetingon May 1, 2024 at 7:03 am
Kerecis, the company pioneering the use of sustainably sourced fish skin and fatty acids in cellular therapy and tissue regeneration and protection, will present two symposiums and 27 abstracts on its ...
- Root canal? Next-gen treatment could involve stem cells, not surgeryon April 30, 2024 at 5:00 pm
“Over the past two decades, scientists have come to rely on stem cells for tissue regeneration. We haven’t tapped into that nearly enough in dental medicine,” Sabatini noted. “The standard of care in ...
- Tissue Engineering and Regeneration Market [2028]: Navigating Opportunities and Challengeson April 24, 2024 at 3:11 am
USD 14.57 billion in 2022 and is poised for substantial growth, projecting a Compound Annual Growth Rate (CAGR) of 8.35% through 2028.
- Technion breakthrough for better drug delivery and tissue implantationon April 23, 2024 at 2:11 pm
Researchers develop ultrasound for non-invasive method for bio-printing live cells and tissues deep within the body.
- New small molecule helps scientists study regenerationon April 23, 2024 at 9:23 am
Regenerating damaged tissues or organs has been a dream of scientists for decades. Now, researchers at the FMI and Novartis Biomedical Research have discovered a new molecule that activates a protein ...
- Zebrafish Immune System Linked to Ability To Regenerate Damaged Heart Tissueon April 22, 2024 at 1:59 am
A heart attack will leave a permanent scar on a human heart, yet other animals, including zebrafish, can clear cardiac scar tissue and regrow damaged muscle. A new study sheds light on the molecular ...
via Bing News