These differences apply even after the doctor has seen the patient
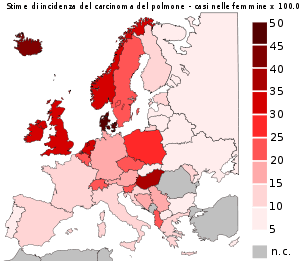
Mathematical prediction models are better than doctors at predicting the outcomes and responses of lung cancer patients to treatment, according to new research presented April 20, 2013, at the 2nd Forum of the European Society for Radiotherapy and Oncology (ESTRO).
These differences apply even after the doctor has seen the patient, which can provide extra information, and knows what the treatment plan and radiation dose will be.
“The number of treatment options available for lung cancer patients are increasing, as well as the amount of information available to the individual patient. It is evident that this will complicate the task of the doctor in the future,” said the presenter, Dr Cary Oberije, a postdoctoral researcher at the MAASTRO Clinic, Maastricht University Medical Center, Maastricht, The Netherlands. “If models based on patient, tumour and treatment characteristics already out-perform the doctors, then it is unethical to make treatment decisions based solely on the doctors’ opinions. We believe models should be implemented in clinical practice to guide decisions.”
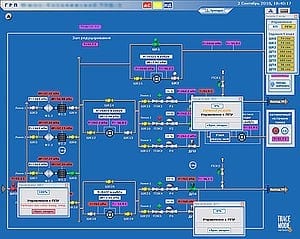
Dr Oberije and her colleagues in The Netherlands used mathematical prediction models that had already been tested and published. The models use information from previous patients to create a statistical formula that can be used to predict the probability of outcome and responses to treatment using radiotherapy with or without chemotherapy for future patients.
Having obtained predictions from the mathematical models, the researchers asked experienced radiation oncologists to predict the likelihood of lung cancer patients surviving for two years, or suffering from shortness of breath (dyspnea) and difficulty swallowing (dysphagia) at two points in time: 1) after they had seen the patient for the first time, and 2) after the treatment plan was made. At the first time point, the doctors predicted two-year survival for 121 patients, dyspnea for 139 and dysphagia for 146 patients. At the second time point, predictions were only available for 35, 39 and 41 patients respectively.
For all three predictions and at both time points, the mathematical models substantially outperformed the doctors’ predictions, with the doctors’ predictions being little better than those expected by chance.
The researchers plotted the results on a special graph on which the area below the plotted line is used for measuring the accuracy of predictions; 1 represents a perfect prediction, while 0.5 represents predictions that were right in 50% of cases, i.e. the same as chance. They found that the model predictions at the first time point were 0.71 for two-year survival, 0.76 for dyspnea and 0.72 for dysphagia. In contrast, the doctors’ predictions were 0.56, 0.59 and 0.52 respectively.
The models had a better positive predictive value (PPV) – a measure of the proportion of patients who were correctly assessed as being at risk of dying within two years or suffering from dyspnea and dysphagia – than the doctors. The negative predictive value (NPV) – a measure of the proportion of patients that would not die within two years or suffer from dyspnea and dysphagia – was comparable between the models and the doctors.
“This indicates that the models were better at identifying high risk patients that have a very low chance of surviving or a very high chance of developing severe dyspnea or dysphagia,” said Dr Oberije.
The researchers say that it is important that further research is carried out into how prediction models can be integrated into standard clinical care. In addition, further improvement of the models by incorporating all the latest advances in areas such as genetics, imaging and other factors, is important. This will make it possible to tailor treatment to the individual patient’s biological make-up and tumour type
“In our opinion, individualised treatment can only succeed if prediction models are used in clinical practice. We have shown that current models already outperform doctors. Therefore, this study can be used as a strong argument in favour of using prediction models and changing current clinical practice,” said Dr Oberije.
The Latest Bing News on:
Mathematical prediction models
- Who is Allan Lichtman and how does he predict the presidential race with such accuracy?on May 8, 2024 at 8:36 am
Known as the presidential prognosticator, this American University professor has a strong record of predicting who might win the White House.
- 'Mathematical microscope' reveals novel, energy-efficient mechanism of working memory that works even during sleepon May 8, 2024 at 2:01 am
UCLA Health researchers have discovered a mechanism that creates memories while reducing metabolic cost, even during sleep. This efficient memory occurs in a part of the brain that is crucial for ...
- Meta’s new multi-token prediction makes AI models up to 3X fasteron May 6, 2024 at 4:34 pm
Multi-token prediction instructs the LLM to predict several future tokens from each position in the training corpora at the same time.
- Joe Biden’s Terrible Approval Rating May Not Matteron May 6, 2024 at 3:00 am
With his approval rating averaging a paltry 38.7 percent over the last three months, it is impossible for Biden to run a “Morning Again in America” reelection campaign, no matter what the jobs numbers ...
- New model may explain 'cosmic glitch,' where gravity weakens at edge of universe, scientists sayon May 2, 2024 at 1:45 am
A new model could explain the cosmic glitch at the edge of the expanding universe, where gravity weakens by about a per cent, according to new research.
- New computer algorithm supercharges climate models and could lead to better predictions of future climate changeon May 1, 2024 at 11:00 am
Earth System Models—complex computer models that describe Earth processes and how they interact—are critical for predicting future climate change. By simulating the response of our land, oceans and ...
- A 'cosmic glitch' in gravity: New model may explain strange behavior on a cosmic scaleon May 1, 2024 at 8:04 am
A group of researchers at the University of Waterloo and the University of British Columbia have discovered a potential "cosmic glitch" in the universe's gravity, explaining its strange behavior on a ...
- AI Chatbots Need Large Language Models. Here's What to Know About LLMson April 24, 2024 at 4:00 pm
Generative AI tools are constantly refining their understanding of words to make better predictions. Some, including Google's Lumiere and OpenAI's Sora, are even learning to generate images, video and ...
- A new diagnostic model offers hope for Alzheimer'son April 10, 2024 at 5:00 pm
A new mathematical model offers hope for better prediction and treatment of Alzheimer's disease. Most mathematical models of Alzheimer's are theoretical, focusing on short term molecular and ...
The Latest Google Headlines on:
Mathematical prediction models
[google_news title=”” keyword=”Mathematical prediction models” num_posts=”10″ blurb_length=”0″ show_thumb=”left”] [/vc_column_text]The Latest Bing News on:
Prediction models
- Google DeepMind debuts AlphaFold 3 model for predicting the structure of biomoleculeson May 8, 2024 at 3:43 pm
Google’s AlphaFold family of artificial intelligence models can significantly speed up the task by automating manual work for scientists. The first iteration of the model that the company debuted in ...
- InnovationRx: Deepmind Unveils Its New Protein-Folding AI Model AlphaFold 3on May 8, 2024 at 2:17 pm
InnovationRx is your weekly digest of healthcare news. To get it in your inbox, subscribe here.
- Researchers develop falls prediction model using health records to predict patients' risk of falling in the UKon May 8, 2024 at 1:11 pm
Patients' risk of falling in the next 12 months could be predicted from their NHS data using a newly developed calculator.
- Braves vs. Red Sox prediction: MLB odds, picks, betson May 8, 2024 at 12:20 pm
Red Sox vs. Braves is a sneaky underrated interleague matchup. Boston has the best pitching staff in the American League, while Atlanta still boasts a roster talented enough to win another World ...
- Yankees vs. Astros prediction: MLB picks, odds for Wednesdayon May 8, 2024 at 12:00 pm
The Yankees are barely keeping pace with the Orioles and looking for another solid start from lefty Carlos Rodon.
- Google DeepMind’s new AI can model DNA, RNA, and ‘all life’s molecules’on May 8, 2024 at 10:38 am
DeepMind says the new model shows a 50 percent improvement in prediction accuracy compared to its previous models. “With AlphaFold 2, it was a big milestone moment in structural biology and has ...
- Who is Allan Lichtman and how does he predict the presidential race with such accuracy?on May 8, 2024 at 8:36 am
Known as the presidential prognosticator, this American University professor has a strong record of predicting who might win the White House.
- Multi Token Prediction Increases AI Model Speed Three Times, Says Metaon May 6, 2024 at 10:07 pm
Training language models to predict multiple tokens at once results in better sample efficiency, says researchers at Meta. Large language models like Llama and ChatGPT are usually trained for the next ...
- Meta’s new multi-token prediction makes AI models up to 3X fasteron May 6, 2024 at 4:34 pm
Multi-token prediction instructs the LLM to predict several future tokens from each position in the training corpora at the same time.
- Phillies vs. Giants odds, line, score prediction, start time: 2024 MLB picks, May 6 best bets by proven modelon May 6, 2024 at 11:07 am
SportsLine's model simulated Monday's New York Giants vs. Philadelphia Phillies game 10,000 times and released its MLB picks, predictions and best bets ...
The Latest Google Headlines on:
Prediction models
[google_news title=”” keyword=”prediction models” num_posts=”10″ blurb_length=”0″ show_thumb=”left”]