Scientists at BC Children’s Hospital and the University of British Columbia have developed a gene therapy that programs a type of immune cell called T regulatory cells (Tregs) to protect transplanted tissues from rejection by the patient’s immune system.
The proof-of-concept study is published today in the Journal of Clinical Investigation print issue.
“With further research, Tregs could be given as a living drug to prevent immune attack of transplanted cells and organs,” says Dr. Megan Levings, the study’s principal investigator.
Dr. Levings is a scientist at the Child & Family Research Institute (CFRI) at BC Children’s Hospital where she leads the Childhood Diseases research theme, and she is a professor in the Department of Surgery at the University of British Columbia (UBC).
“This exciting discovery is the first step towards testing these cells in humans undergoing transplantation,” says Dr. Levings.
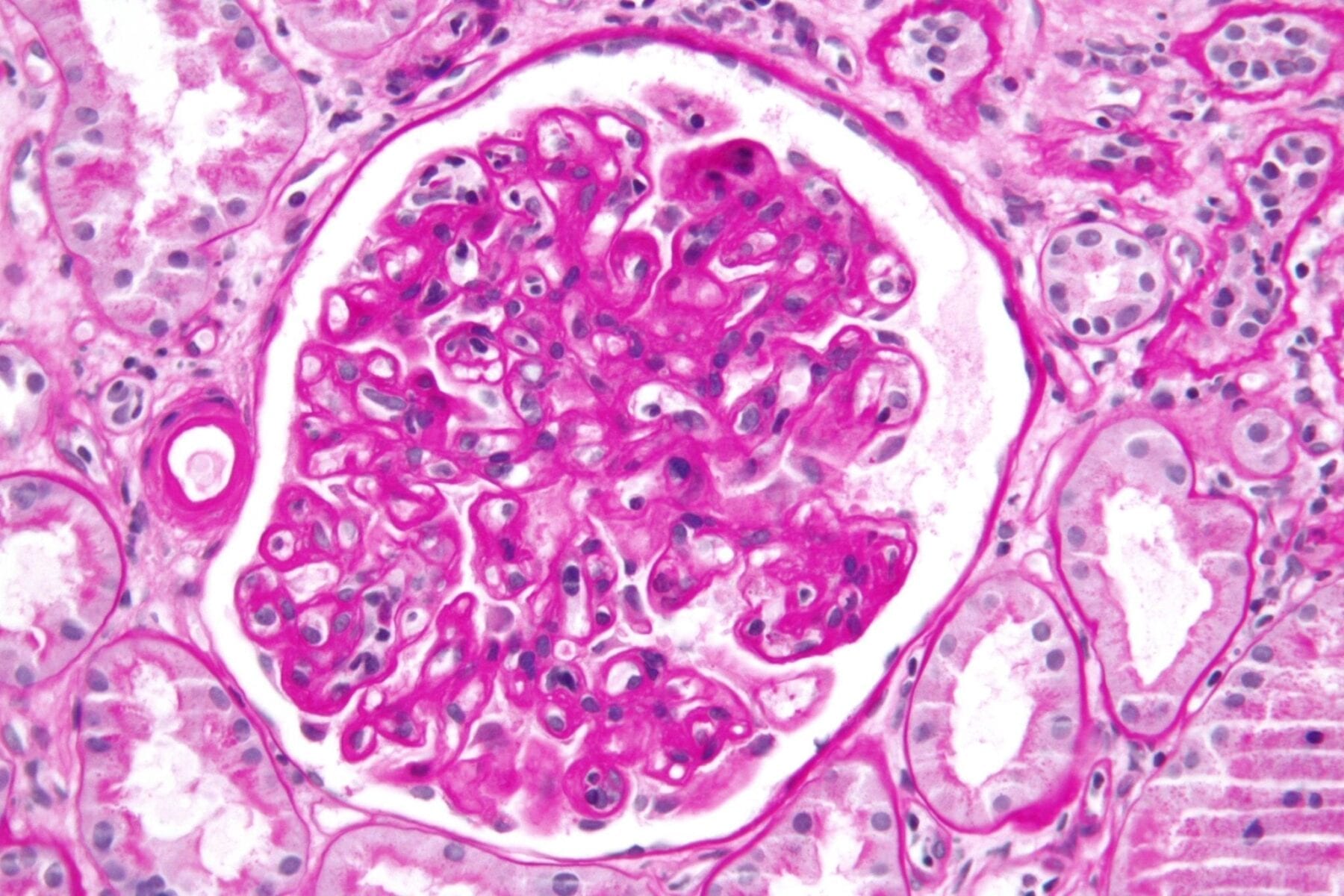
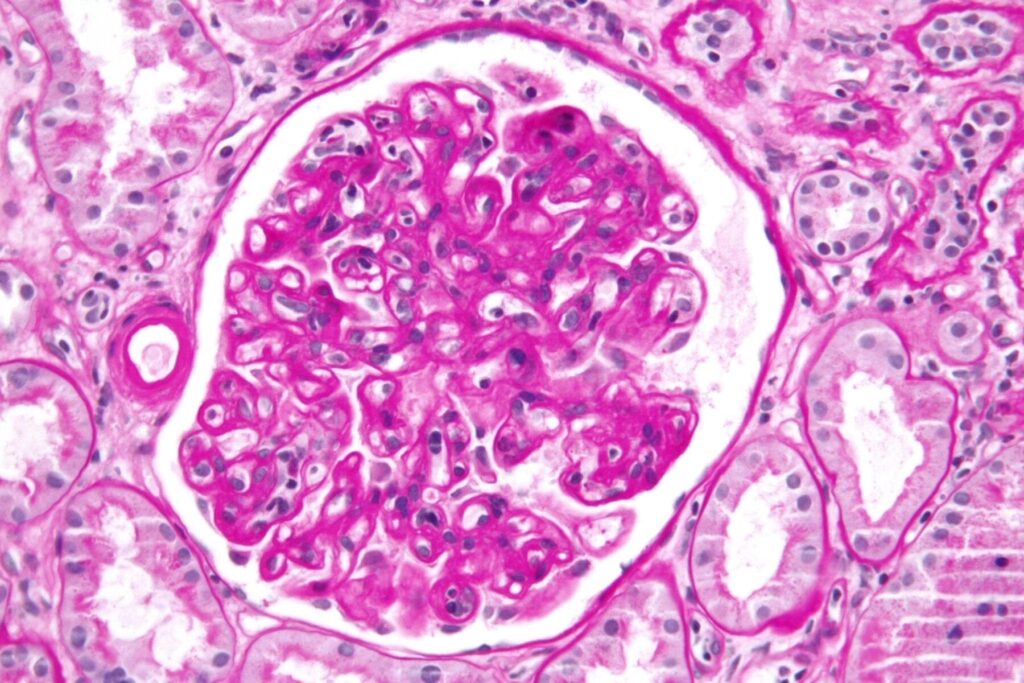
After transplantation, the patient’s body sometimes identifies the transplanted tissue as foreign and mounts an immune attack against it. For this reason, most transplant patients must take immune-suppressing medications for the rest of their lives.
In 2014, there were 2,433 solid organs transplanted in Canada and from 2010-2015, there were 52 pediatric solid organ transplants performed in British Columbia.
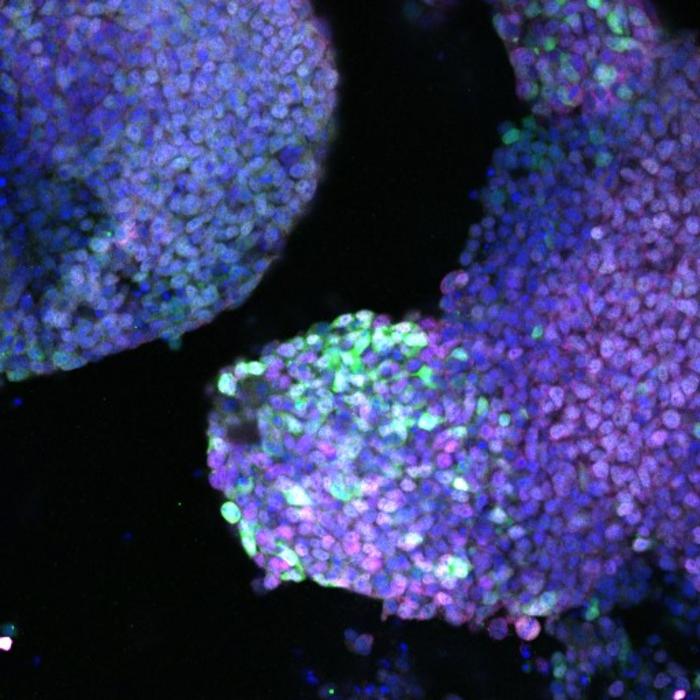
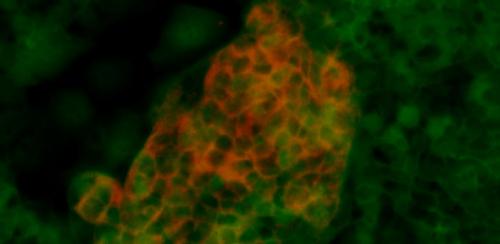
For this study, the scientists removed Tregs from blood donated by volunteers to the Canadian Blood Services. The scientists built a gene that makes a protein called CAR (chimeric antigen receptor). They used a harmless virus to insert the CAR gene into Tregs, which programmed the cells to recognize specific proteins commonly found on the surface of transplanted tissues. The normal role of Tregs is to turn off the immune response and prevent an immune response to healthy tissues. The scientists did a series of experiments that proved the modified Tregs could recognize transplanted tissues and protect them from the immune system.
A related concept is used in a type of cancer treatment called immunotherapy where the patient’s own immune cells are genetically programmed with the CAR gene to mount an immune response against tumour cells.
“We took this approach from cancer immunotherapy and we used it for the opposite purpose – to turn off unwanted immune responses,” says Dr. Levings.
“It’s a whole new age in medicine, and we’re doing cutting edge work right here in BC,” says Dr. Katherine MacDonald, the study’s first author. The research was the basis of Dr. MacDonald’s doctoral thesis while she was a UBC trainee supervised by Dr. Levings at CFRI.
“With this finding, it opens up the possibility to build a gene for any disease where the immune system is overactive,” says Dr. MacDonald.
This includes autoimmune diseases, which develop when the immune system destroys healthy tissues such as the insulin-producing cells of the pancreas in Type 1 diabetes or cells of the intestinal lining in inflammatory bowel disease.
The researchers say a decade of further work is needed to develop safe and targeted treatments using modified Tregs.
Learn more: BC scientists engineer immune cells to protect organs from transplant rejection
The Latest on: Transplant rejection
[google_news title=”” keyword=”transplant rejection” num_posts=”10″ blurb_length=”0″ show_thumb=”left”]
via Google News
The Latest on: Transplant rejection
- Genetic and Genomic Approaches to the Detection of Heart Transplant Rejectionon April 26, 2024 at 5:00 pm
Because HLA matching between donor and recipient is not possible, patients are at risk for rejection after transplant, despite treatment with immunosuppressive medications such as tacrolimus and ...
- Noninvasive Methods to Assess the Risk of Kidney Transplant Rejectionon April 24, 2024 at 5:00 pm
In stable kidney transplant patients ... with a labelled secondary antibody Helpful in predicting the risk of acute rejection Effective in tailoring immunosuppressive therapy Relatively easy ...
- New clinical trial aims to investigate skin patches to spot lung transplant rejectionon April 18, 2024 at 5:00 pm
Involving 152 patients, the SENTINEL trial aims to cut lung transplant rejection by up to 50% A new clinical trial being led by the University of Oxford’s Surgical Trial Units in collaboration with ...
- Researchers probe immune microenvironment to prevent pediatric liver transplant rejectionon April 17, 2024 at 6:46 am
Children with liver transplants must take immunosuppressant medications for life. To maintain tolerance of the transplanted liver, doctors treat transplant rejection and conduct ongoing maintenance ...
- ‘Crucial’ new skin patches that develop into a rash can alert doctors to organ transplant rejectionon April 15, 2024 at 5:07 pm
SKIN patches could halve rates of deadly organ rejection in transplant patients, hope scientists running an NHS trial. Around 4,500 Brits have organ transplants each year but the body rejects them ...
- Children’s Hospital Los Angeles researchers probe immune microenvironment to prevent pediatric liver transplant rejectionon April 11, 2024 at 5:00 pm
coauthored a study to develop an approach to predict and prevent liver transplant rejection in children. Children with liver transplants must take immunosuppressant medications for life.
- Kidney transplant patients to get ‘double matched blood’ to avoid rejectionon April 8, 2024 at 5:00 pm
Scientists are to double match blood intended for use for kidney transplant patients in a bid to make sure their donated kidney is less likely to be rejected. As well as ensuring that blood is ...
- Natera Announces New Data From Two Studies Extending the Clinical Validation of Its Prospera™ Heart dd-cfDNA Test for Heart Transplant Recipientson April 8, 2024 at 5:01 am
The DTRT-2 (DNA-Based Transplant Rejection Test) study, published recently in Pediatric Transplantation, was sponsored by the National Institutes of Health (NIH). A total of 487 samples from 160 ...
via Bing News