Researchers have made a significant first step with newly engineered biomaterials for cell transplantation that could help lead to a possible cure for Type 1 diabetes, which affects about 3 million Americans.
Georgia Tech engineers and Emory University clinicians have successfully engrafted insulin-producing cells into a diabetic mouse model, reversing diabetic symptoms in the animal in as little as 10 days.
The research team engineered a biomaterial to protect the cluster of insulin-producing cells – donor pancreatic islets – during injection. The material also contains proteins to foster blood vessel formation that allow the cells to successfully graft, survive and function within the body.
“It’s very promising,” said Andrés Garcia, Georgia Tech professor of mechanical engineering. “There is a lot of excitement because not only can we get the islets to survive and function, but we can also cure diabetes with fewer islets than are normally needed.”
The research article – a partnership with Emory’s Dr. Robert Taylor and Dr. Peter Thule that was funded in part by theJDRF, the leading global organization funding Type 1 diabetes research – will be published in the June issue of the journal Biomaterials.
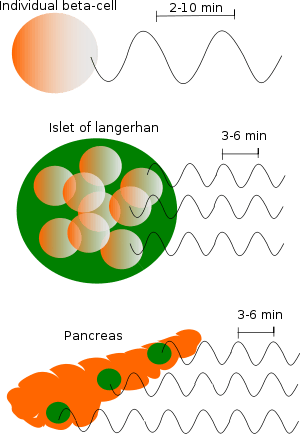
Organizations such as JDRF are dedicated to finding a cure for Type 1 diabetes, a chronic disease that occurs when the pancreas produces little or no insulin, a hormone that allows the transport of sugar and other nutrients into tissues where they are converted to energy needed for daily life.
Pancreatic islet transplantation re-emerged as a promising therapy in the late 1990s. Patients with diabetes typically find it difficult to comply with multiple daily insulin injections, which only partially improve long-term outcomes. Successful islet transplantation would remove the need for patients to administer insulin. While islet transplantation trials have had some success, and control of glucose levels is often improved, diabetic symptoms have returned in most patients and they have had to revert to using some insulin.
Unsuccessful transplants can be attributed to several factors, researchers say. The current technique of injecting islets directly into the blood vessels in the liver causes approximately half of the cells to die due to exposure to blood clotting reactions. Also, the islets – metabolically active cells that require significant blood flow – have problems hooking up to blood vessels once in the body and die off over time.
Georgia Tech and Emory researchers engineered a hydrogel, a material compatible with biological tissues that is a promising therapeutic delivery vehicle. This water-swollen, cross-linked polymer surrounds the insulin-producing cells and protects them during injection. The hydrogel containing the islets was delivered to a new injection site on the outside of the small intestine, thus avoiding direct injection into the blood stream.
Once in the body, the hydrogel degrades in a controlled fashion to release a growth factor protein that promotes blood vessel formation and connection of the transplanted islets to these new vessels. In the study, the blood vessels effectively grew into the biomaterial and successfully connected to the insulin-producing cells.
Four weeks after the transplantation, diabetic mice treated with the hydrogel had normal glucose levels, and the delivered islets were alive and vascularized to the same extent as islets in a healthy mouse pancreas. The technique also required fewer islets than previous transplantation attempts, which may allow doctors to treat more patients with limited donor samples. Currently, donor cells from two to three cadavers are needed for one patient.
While the new biomaterial and injection technique is promising, the study used genetically identical mice and therefore did not address immune rejection issues common to human applications. The research team has funding from JDRF to study whether an immune barrier they created will allow the cells to be accepted in genetically different mice models. If successful, the trials could move to larger animals.
“We broke up our strategy into two steps,” said Garcia, a member of Georgia Tech’s Petit Institute for Bioengineering and Bioscience. “We have shown that when delivered in the material we engineered, the islets will survive and graft. Now we must address immune acceptance issues.”
The Latest Bing News on:
Diabetes mellitus type 1
- Europe’s amputation crisis, diabetes experts call for urgent new screening programson April 30, 2024 at 7:14 pm
Europeans suffer 100,000 amputations a year because of the escalating issue of ‘diabetic foot’. Diabetes already burdens health systems, but without more frequent monitoring programmes, experts warn ...
- Ancient grains show promise for type 2 diabeteson April 28, 2024 at 11:00 pm
Image Credit: windcoast / Shutterstock Furthermore, with a sole exception, the health outcomes of ancient grains consumption in type 1 diabetes mellitus (T1DM) remain poorly understood. This review ...
- Affordability of Lirafit expected to significantly impact Indian diabetes market: Alok Malikon April 28, 2024 at 6:33 am
Liraglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) that has been shown to effectively lower glycemic parameters, promote weight reduction, and ensure cardiovascular safety in ...
- Signs and Symptoms of Diabetes Insipiduson April 24, 2024 at 9:30 am
Diabetes insipidus is a rare condition that causes extreme thirst and frequent urination. Headache and double vision are also possible symptoms.
- Type 1 Diabeteson April 18, 2024 at 5:00 pm
What Is Type 1 Diabetes? Type 1 diabetes is a condition in which your immune system destroys insulin-making cells (beta cells) in your pancreas. That means your body can't make enough insulin or ...
- Ask A Doctor: How Do You Develop Diabetes Type 1?on April 6, 2024 at 12:02 pm
Diabetes type—1 is insulin-dependent diabetes mellitus, in which there is little or no insulin production from pancreas. Insulin is a hormone needed to allow sugar to enter cells to produce energy.
- Stem cell therapy for type 1 diabetes mellituson September 14, 2022 at 6:17 pm
The use of stem cells in regenerative medicine holds great promise for the cure of many diseases, including type 1 diabetes mellitus (T1DM). Any potential stem-cell-based cure for T1DM should ...
- Diabetes Mellitus Type 1 Newson August 9, 2022 at 5:00 pm
Increase in New-Onset Type 1 Diabetes in Kids During Pandemic The early days of the COVID-19 pandemic saw an increase in new-onset pediatric diabetes and DKA, while children with pre-existing ...
- Diabetes Mellitus Type 1 Newson August 18, 2021 at 7:13 pm
Too Little Sleep Raises Health Risks for Teens With T1D Sleeping for more than 7 hours at night may improve cardiometabolic health in patients with type 1 diabetes, especially teenagers ...
- Type 1 Diabeteson June 17, 2020 at 12:19 pm
Type 1 diabetes mellitus describes a condition where the body cannot produce insulin which leads to a very high level of blood sugar and associated complications. The condition, which usually ...
The Latest Google Headlines on:
Diabetes mellitus type 1
[google_news title=”” keyword=”Diabetes mellitus type 1″ num_posts=”10″ blurb_length=”0″ show_thumb=”left”]
The Latest Bing News on:
Cure for type 1 diabetes
- Potential Targeted Therapy for Type I Diabetes: Monoclonal Antibodieson May 2, 2024 at 12:30 am
Innovative study on mice leads to a potential targeted monoclonal antibody therapy to manage Type I diabetes. Study highlights need for human version of antibody.
- Bill improving Type 1 diabetes education for students, families moves to Illinois Houseon May 1, 2024 at 2:15 pm
A bill heading to the Illinois House floor could help students and families better understand the signs and symptoms of Type 1 diabetes.
- Experimental monoclonal antibody prevents and reverses clinical type 1 diabetes in miceon April 30, 2024 at 11:47 am
Scientists at Johns Hopkins Medicine say that an experimental monoclonal antibody drug called mAb43 appears to prevent and reverse the onset of clinical type 1 diabetes in mice, and in some cases, to ...
- Experimental Drug “Hides” Pancreas Cells in Type 1 Diabetes Mouse Modelson April 29, 2024 at 5:00 pm
raise the possibility of a new drug for type 1 diabetes, an autoimmune condition that affects about 2 million American children and adults and has no cure or means of prevention. Unlike type 2 ...
- Bioengineer explores new approach to diabetes treatmenton April 29, 2024 at 12:31 pm
The chair of the Bioengineering Department at The University of Texas at Arlington is working on an invention that will allow for better treatment of Type 1 diabetes patients.
- Raising awareness and money to end type 1 diabeteson April 29, 2024 at 10:00 am
C Juvenile Diabetes Research Foundation. Find out how these families are helping find a cure for Type 1 diabetes — and how you can help too.
- Use of insulin pumps tied to preterm delivery, fetal overgrowth in pregnant women with type 1 diabetes: Studyon April 28, 2024 at 9:00 am
Denmark: A recent analysis of EVOLVE Study Cohort has shown a higher risk of large for gestational age (LGA) offspring and preterm delivery with the insulin pump treatment (versus multiple ...
- Breakthrough: Rare Gene Mutation Offers Clues to Preventing Type 1 Diabeteson April 25, 2024 at 8:39 pm
A unique genetic mutation in two siblings – that has never been seen in anyone else – has been discovered by UK researchers at the University of Exeter, pointing the way towards new treatment options ...
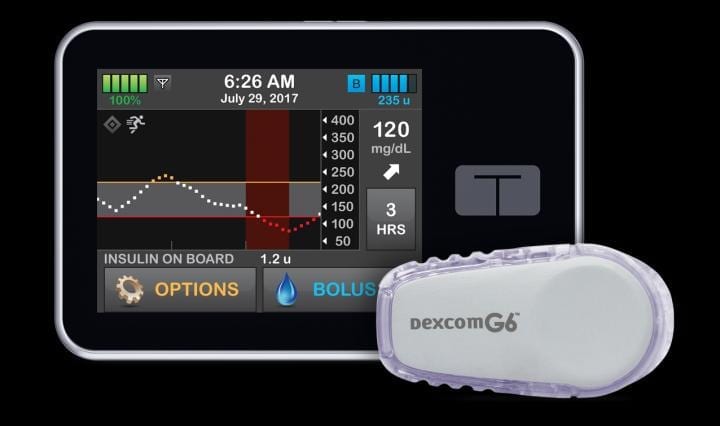
- Study shows hybrid pumps work very well in type 1 diabeteson April 24, 2024 at 11:12 am
Blood sugar levels improve when adults with type 1 diabetes use modern insulin pumps. These are the findings of a study conducted at the University of Gothenburg. Patients are also overwhelmingly ...
- Siblings with unique gene mutation offer insights into type 1 diabetes treatmenton April 20, 2024 at 10:51 pm
Two siblings who have the only known mutations in a key gene anywhere in the world have helped scientists gain new insights that could help progress the search for new treatments in type 1 diabetes.
The Latest Google Headlines on:
Cure for type 1 diabetes
[google_news title=”” keyword=”cure for type 1 diabetes” num_posts=”10″ blurb_length=”0″ show_thumb=”left”]