Credit: Rachel Qu, Anna Stokolosa, Charlotte Culip
Traditional surgery to reshape a nose or ear entails cutting and suturing, sometimes followed by long recovery times and scars. But now, researchers have developed a “molecular surgery” process that uses tiny needles, electric current and 3D-printed molds to quickly reshape living tissue with no incisions, scarring or recovery time. The technique even shows promise as a way to fix immobile joints or as a noninvasive alternative to laser eye surgery.
The researchers will present their results today at the American Chemical Society (ACS) Spring 2019 National Meeting & Exposition. ACS, the world’s largest scientific society, is holding the meeting here through Thursday. It features nearly 13,000 presentations on a wide range of science topics.
“We envision this new technique as a low-cost office procedure done under local anesthesia,” says Michael Hill, Ph.D., one of the project’s principal investigators, who will discuss the work at the meeting. “The whole process would take about five minutes.”
Hill, who is at Occidental College, became involved in this project when Brian Wong, M.D., Ph.D., who is at the University of California, Irvine, asked for help in developing a noninvasive technique to reshape cartilage. Such a method would be useful for cosmetic surgery procedures, such as making a nose more attractive. But the method also could help fix problems, such as a deviated septum, or conditions for which no good treatments exist, such as joint contractures caused by stroke or cerebral palsy. Having suffered through painful deviated septum surgery himself, Hill understands what patients go through, and was excited to join a project to develop a better strategy.
Wong was already an expert in one alternative technique that uses an infrared laser to heat cartilage, making it flexible enough to reshape. “The problem is, that technique is expensive, and it’s hard to heat the cartilage enough so that it’s malleable without killing the tissue,” Hill says. To find a more practical approach, Wong’s team began experimenting with passing current through cartilage to heat it up. The method indeed allowed them to reshape tissue, but, curiously, not by warming it. Wong turned to Hill to determine just how the new method was working and to refine it to prevent tissue damage.
Cartilage is made up of tiny rigid fibers of collagen loosely woven together by biopolymers. Its structure resembles spaghetti that’s been randomly dumped on a counter, with the individual strands tied together with thread. “If you picked it up, the strands wouldn’t fall apart, but it would be floppy,” Hill says. Cartilage also contains negatively charged proteins and positively charged sodium ions. Cartilage with a greater density of these charged particles is stiffer than cartilage with a lower charge density.
Hill’s group discovered that passing current through cartilage electrolyzes water in the tissue, converting the water into oxygen and hydrogen ions, or protons. The positive charge of the protons cancels out the negative charge on the proteins, reducing charge density and making the cartilage more malleable. “Once the tissue is floppy,” he says, “you can mold it to whatever shape you want.”
The team tested the method on a rabbit whose ears normally stand upright. They used a mold to hold one ear bent over in the desired new shape. If they had then removed the mold without applying a current, the rabbit’s ear would have sprung back into its original upright position, just like a human ear would. But by inserting microneedle electrodes into the ear at the bend and pulsing current through them with the mold in place, they briefly softened the cartilage at the bend site without damage. Turning off the current then allowed the cartilage to harden in its new shape, after which the mold was removed.
To achieve this outcome with traditional methods, a surgeon would have to cut through the skin and cartilage and then stick the pieces back together. That can lead to formation of scar tissue at the joint. That scar tissue must sometimes be removed in subsequent operations, Hill says. By avoiding this mechanical damage to the cartilage, the molecular surgery technique causes no scarring and no pain.
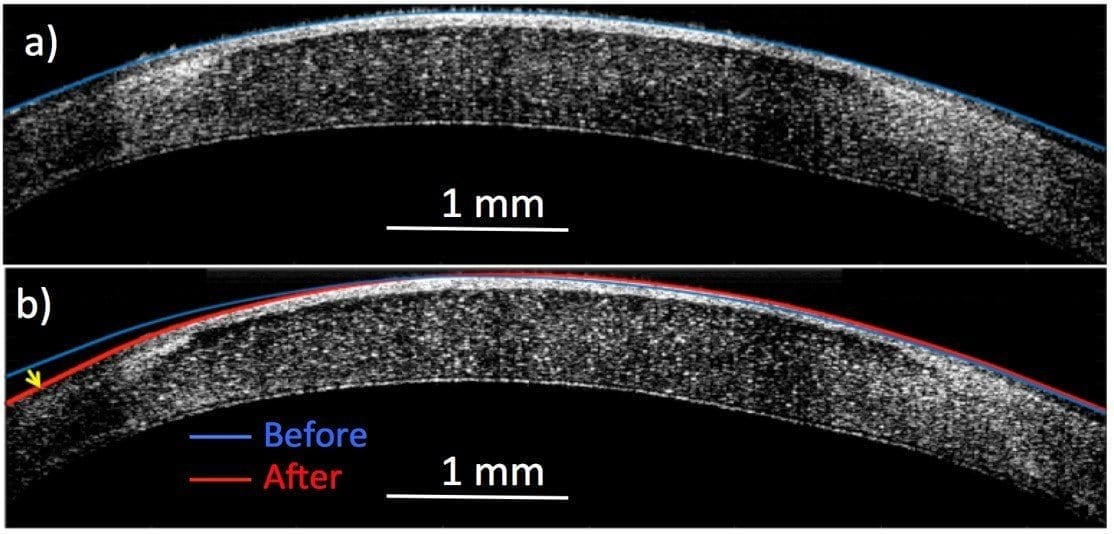
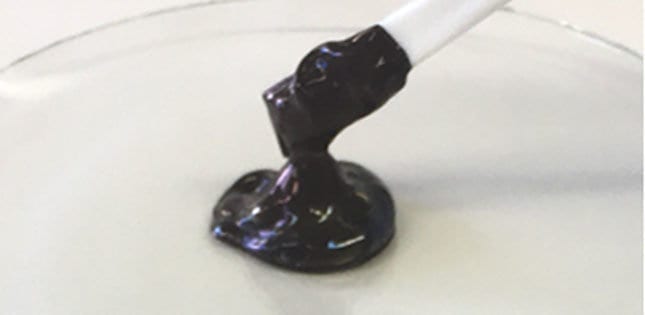
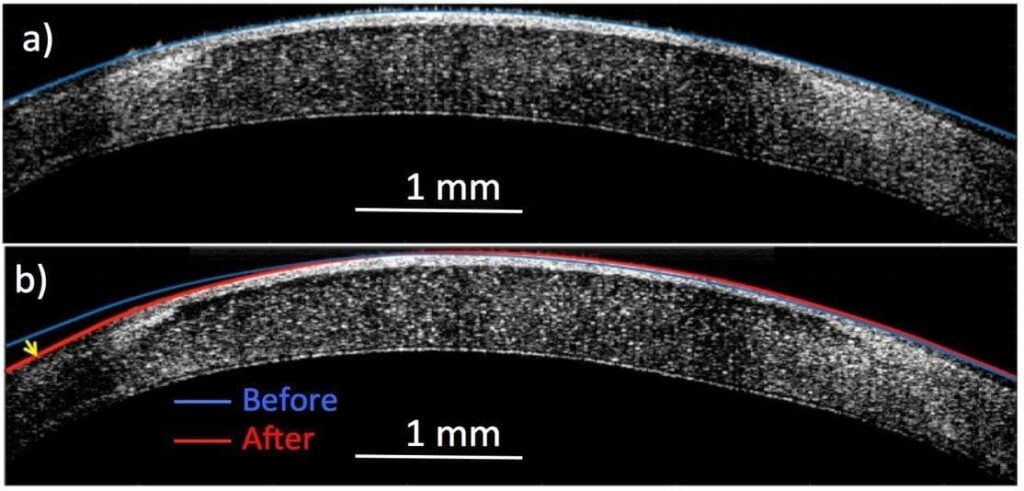
The researchers are exploring licensing options for the cartilage technique with medical device companies. They’re also investigating applications in other types of collagen tissue, such as tendons and corneas. In an eye, cornea shape affects vision, with too much curvature causing nearsightedness, for example. Many hurdles must be overcome before this method could be used to correct a person’s vision, but preliminary animal experiments have had promising results. The researchers used a 3D printer to make a contact lens. After painting electrodes on it, they put the contact lens on the eye. Applying current allowed them to temporarily soften the cornea and change its curvature.
Learn more: ‘Molecular surgery’ reshapes living tissue with electricity but no incisions
The Latest on: Molecular surgery
[google_news title=”” keyword=”molecular surgery” num_posts=”10″ blurb_length=”0″ show_thumb=”left”]
via Google News
The Latest on: Molecular surgery
- Blood Test Detects Knee Osteoarthritis Years Before X-Ray Visibilityon April 27, 2024 at 3:04 pm
Kraus and colleagues have focused on developing molecular biomarkers that can be used for both clinical diagnostic purposes and as a research tool to aid in the development of effective drugs. In ...
- AI-powered test predicts knee osteoarthritis 8 years before X-rayon April 27, 2024 at 10:33 am
A new biomarker test successfully predicted the early onset of knee osteoarthritis years ahead of noticeable signs.
- Blood test predicts knee osteoarthritis eight years before tell-tale signs of the diseaseon April 26, 2024 at 10:53 pm
A blood test successfully predicted knee osteoarthritis at least eight years before tell-tale signs of the disease appeared on x-rays, Duke Health researchers report.
- Ruling: Iowa state auditor must provide more evidence to justify withholding emailson April 26, 2024 at 5:45 pm
The state auditor's office must do more to justify its decision to withhold from public release emails between his office and two journalists, the Iowa Supreme Court ruled.
- Blood test finds knee osteoarthritis up to 8 years before it appears on X-rayson April 26, 2024 at 11:00 am
Detecting knee osteoarthritis with a blood test up to eight years before it appears on X-rays -- as researchers have done -- could lead to therapies that delay disease progression and restore joint ...
- Blood Test Detects Knee Osteoarthritis 8 Years Before X-Rayson April 26, 2024 at 11:00 am
Early detection of knee osteoarthritis could lead to therapies that slow progression and restore joint health. A blood test successfully predicted knee osteoarthritis at least eight years before ...
- Aisley races to a bright future after recovering from rare brain tumoron April 26, 2024 at 5:55 am
Aisley’s pediatrician referred her to Seattle Children’s, where an MRI revealed a life-threatening tumor that was pushing her brain to one side.
- Blood test can detect signs of knee condition 8 years before X-rayson April 25, 2024 at 5:00 pm
Kraus and her team focused on developing molecular biomarkers that can be used for both clinical diagnostic purposes as well as a research tool to help develop effective drugs. In previous studies, ...
- These Are The Biotechs Showing Up At The Biggest Cancer Meeting Of The Year (Oral Presentations)on April 25, 2024 at 2:49 pm
Meeting of ASCO is a major event for clinicians and researchers in the field of oncology. Explore more details here.
- 14 recent scientific breakthroughson April 24, 2024 at 8:40 am
T cells are integral in the immune system but can become "dysfunctional inside tumors." "The approval of Amtagvi represents the culmination of scientific and clinical research efforts leading to a ...
via Bing News