“A good scalpel makes a better surgeon. Good communication makes a better doctor.”
– Dr. Josh Umbehr
The future of medicine in the U.S. is clear. The days of the “do more, bill more” model of reimbursement are numbered as they have produced one of the most inefficient healthcare systems in the world. While there are many unknowns regarding the future model, one thing is crystal clear — highly effective communication will separate the winners from the losers.
The quantum improvement in the depth and breadth of communication seen in the consumer Internet and in the consumerization of the enterprise (iPhones, Yammer, etc.) has yet to fully impact healthcare. With healthcare representing nearly 20% of the economy, the stakes are so high that it is inevitable that communications will be a key driver separating the winners from the losers as the tectonic shifts in the landscape shake out. This will usher in an array of new technology entrants similar to consumer and enterprise arenas disrupting ineffective and expensive communication methods of the past. The stars are aligning to make this happen.
“I don’t think you can overstate the importance of communication in clinical care. Even with devices, robotics, genomics and personalized care, it all rests, and depends on, clear communication.”
– Dr. Wendy Sue Swanson, MD, MBE, FAAP
The Individual (aka the Patient) is the Most Important Member of the Care Team
It’s long been said that the most important member of the care team is the individual (or their family member).
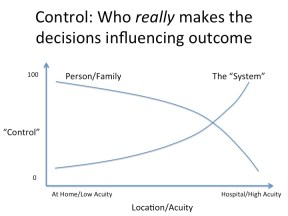
Quite simply, in a world where one is compensated on value and outcome, it’s nearly impossible to have success without recognizing the importance of the patient. Consider the diagram in this article. It is clear and appropriate that the “system” — i.e., the collection of healthcare providers — is in control of decisions that drive outcomes in high acuity cases such as when one is unconscious in the hospital. In contrast, in low acuity situations such as managing a chronic condition, the individual and/or their family are clearly in control of actions that will drive the ultimate outcome. Whether adhering to an exercise, diet or prescription plan, the patient/family plays the central role in determining the outcome.
The importance of this can’t be overemphasized given that 75% of healthcare spend results from chronic conditions. Decisions made while a condition is in low acuity can rapidly lead to high acuity flare ups that drive large medical bills. As Dr. Swanson states, “the steering wheel should be attended by the patient.” After all, 99+% of an individual’s life is spent away from healthcare providers and no one else besides them is in the driver’s seat.
It is a good thing that there has been great focus put on improving communication between healthcare professionals through standards and incentives related to the new models being driven by private and federal insurance programs. The Patient Centered Medical Home and the Accountable Care Organizations are the two most high profile of these. However, the communication focus has been about the patient not with the patient. Having worked in and seen literally hundreds of healthIT systems, the fact is the fundamental purpose of the patient as envisioned by these systems is that the “patient” is merely a vessel to attach billing codes to — not a core part of the care team. This legacy approach will prove to be a fatal flaw in the new reimbursement models. Throwing bodies (e.g., care coordinators) at the problem can help, but will be at a disadvantage versus approaches that combine the best of human and technology driven communication methods.
Read more . . .
Bookmark this page for “medical communication” and check back regularly as these articles update on a very frequent basis. The view is set to “news”. Try clicking on “video” and “2” for more articles.