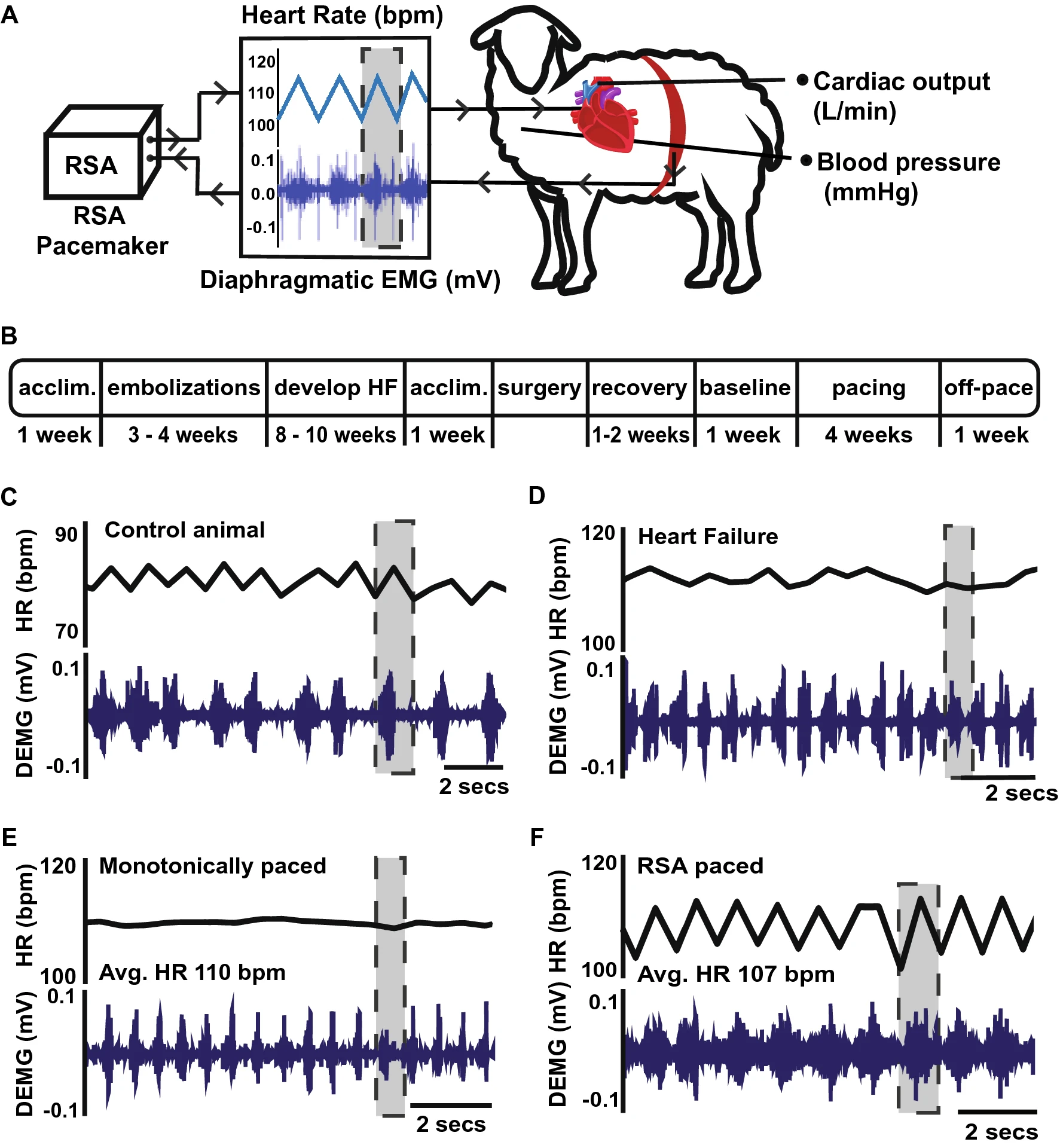
A. Schematic representation of the experimental set-up. Fully instrumented conscious 3–5 year old, outbred, female Romney sheep were paced via the left atrium, 1.5–2.5 V, using a neuron-based pace making device that modulates heart rate in phase with respiration on a breath by breath basis mimicking respiratory sinus arrhythmia (RSA). The device receives diaphragmatic EMG (electromyogram) input to define the phase of inspiration. RSA increases heart rate during inspiration as indicated by the highlighted regions in panels A, C–F Cardiac output was measured on a beat by beat basis using an implantable flow probe attached to the ascending aorta. B Time-line of the six-month experimental protocol. Heart failure with reduced ejection fraction was induced by microembolization and followed by an 8–10 week holding period for chronic heart failure to develop prior to pacing. Following instrumentation and stabilization of hemodynamics parameters, animals were divided into three groups: two were paced (RSA or monotonically) and one not paced (time control) for 4 weeks. This was followed by 1 week off pacing before animals were anaesthetized for baroreflex testing and cardiac tissue collected for post hoc analysis. C Representative raw data traces from a healthy sheep showing native RSA. D A heart failure sheep showing loss of RSA. E A heart failure sheep paced monotonically, showing a stable heart rate. F A heart failure sheep being RSA paced. Note that there was no difference between the mean heart rate of monotonically and RSA paced sheep. Acclim acclimatization to the laboratory; Avg. average; bpm, beats per minute; DEMG diaphragmatic electromyogram; HR heart rate; mV milli Volts
A revolutionary pacemaker that re-establishes the heart’s naturally irregular beat is set to be trialled in New Zealand heart patients this year.
A revolutionary pacemaker that re-establishes the heart’s naturally irregular beat is set to be trialled in New Zealand heart patients this year, following successful animal trials.
“Currently, all pacemakers pace the heart metronomically, which means a very steady, even pace. But when you record heart rate in a healthy individual, you see it is constantly on the move,” says Professor Julian Paton, a lead researcher and director of Manaaki Manawa, the Centre for Heart Research at the University of Auckland.
Manaaki Manawa has led the research and the results have just been published in leading journal Basic Research in Cardiology.
“If you analyse the frequencies within your heart rate, you find the heart rate is coupled to your breathing. It goes up on inspiration, and it goes down on expiration, and that is a natural phenomenon in all animals and humans. And we’re talking about very ancient animals that were on the planet 430 million years ago.”
Twelve years ago, Paton was a member of a group of scientists who decided to investigate the function of this variability. They made a mathematical model that predicted it saved energy. That
made them question why a metronomic heartbeat was used in heart-failure patients who lacked energy. They asked, “Why aren’t we pacing them with this variability?”
All cardiovascular disease patients lose the heart rate variability, which is an early sign that something is going wrong.
“People with high blood pressure, people with heart failure, their heart rate is not being modulated by their breathing. It may be a little bit, but it’s very, very depressed, very suppressed,” Paton says.
“We decided that we would put the heart rate variability back into animals with heart failure and see if it did anything good,” says Paton.
Following positive signals in rats, the latest published research was on a large animal model of heart failure, performed by Dr Julia Shanks and Dr Rohit Ramchandra.
“And the big news is that we believe we have now found a way to reverse heart failure,” Dr Ramchandra says.
Dr Julia Shanks, the research fellow who carried out the research, explains, “There’s nothing really on the market that will cure heart failure. All the drugs will do is make you feel better. They don’t address the issue that you’ve got damaged tissue that’s not contracting as efficiently as it was.
“Our new pacemaker brings back this variability, which of course is natural, in a way you could call it ‘nature’s pacemaker’.”
Dr Ramchandra said, “Currently, pacemakers trigger a metronomically steady beat, but this study shows introducing a natural variation in the heartbeat improves the heart’s ability to pump blood through the body. The other big news is that we get a 20 percent improvement in cardiac output, which is effectively the ability of the heart to pump blood through the body. And 20 percent is a big number.”
“The pacemaker is almost like a bionic device,” says Paton. “It understands the signals from the body that tell the device when we’re breathing in and when we’re breathing out. And then the device has to communicate back to the body and pace the heart up during breathing in and down during breathing out.”
On seeing the results, interventional cardiologist Dr Wil Harrison from Middlemore Hospital remarked: “Very interesting study. We do recognise clinically that permanent pacing is ‘non-physiological’ to a certain degree, and pacing-induced cardiomyopathy is a well-recognised phenomenon. It will be exciting to see if the findings translate over to humans.”
Dr Martin Stiles, a cardiologist from Waikato Hospital, who will lead the trial said: “We typically see improvements in heart function with current pacemakers, but this bionic pacemaker has far exceeded our expectations. This discovery may revolutionise how heart failure patients are paced in the future.”
The next steps are well under way, with plans to recruit patients into a trial planned for later this year in New Zealand. The trial will be supported by Ceryx Medical, a startup company that owns the IP on the unique electronics within the bionic pacemaker.
Original Article: ‘Bionic’ pacemaker reverses heart failure
More from: University of Auckland
The Latest Updates from Bing News & Google News
Go deeper with Bing News on:
Bionic pacemaker
- Accent MRI Pacemaker from St. Jude Medical
The Accent MRI pacemaker, with the Tendril MRI lead, is an MRI conditional system, offering safe performance of a full-body MRI scan on the patient using a 1.5 T (Tesla) field-strength MRI scanner.
- Identity ADx Pacemaker from St. Jude Medical
The Identity ADx pacemaker family, which includes the world's smallest dual-chamber pacemaker, provides clinicians with the most advanced pacemaker technology available, including the ...
- Evaluating MRI-Compatible Pacemakers
As pacemaker technology becomes more complex and sophisticated, new systems present new challenges and more complex modes of failure. The risk of lead failure probably is higher than the risk of ...
- Beware What You Wear With Your Pacemaker or ICD
Relatively weak magnets in consumer products have always posed some risk, usually very low, to the function of pacemakers and implantable cardioverter-defibrillators (ICDs). However, stronger ...
- Pacemaker implant: The lifestyle changes you should expect
If you have an irregular heartbeat that is either too slow or too fast, your cardiologist is likely to recommend you have a pacemaker implant to regulate the heart rhythm. A pacemaker is a small ...
Go deeper with Google Headlines on:
Bionic pacemaker
[google_news title=”” keyword=”bionic pacemaker” num_posts=”5″ blurb_length=”0″ show_thumb=”left”]
Go deeper with Bing News on:
A way to reverse heart failure
- AI technology giving heart failure patients better care, more access to doctors
Revolutionary technology powered by artificial intelligence is giving heart failure patients better care and more access to doctors and the therapies that they need.The technology is helping doctors, ...
- Doxazosin and Congestive Heart Failure
This finding was largely driven by congestive heart failure. The practicing clinician ... rate was unlikely to change in a meaningful enough way by the end of the trial to ethically justify ...
- Heart Failure Deaths Rising, Particularly for Those Under 45
We preselected all newsletters you had before unsubscribing.
- Heart failure mortalities increase — and more
According to JAMA Cardiology, long standing declines in heart failure are reversing. Heart failure death ... At any age a little exercise goes a long way toward improving mood.
- Decline in heart failure deaths has been undone, led by people under 45
Heart failure mortality rates are moving in the wrong direction, a new analysis reports, reversing a decline in ... “We need to move way upstream and think about what we can do a priori to ...
Go deeper with Google Headlines on:
A way to reverse heart failure
[google_news title=”” keyword=”a way to reverse heart failure” num_posts=”5″ blurb_length=”0″ show_thumb=”left”]