Patients at risk of heart attacks and strokes may be spotted earlier thanks to a diagnosis tool that uses near-infrared light to identify high-risk arterial plaques, according to research carried out at WMG, University of Warwick, the Baker Institute and Monash University.
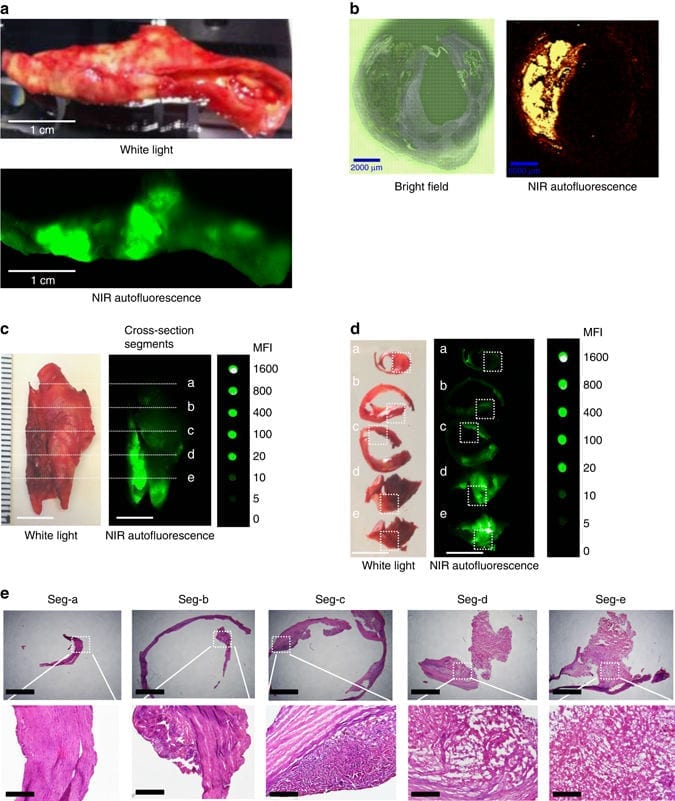
The scientists observed that when they increased the wavelength of the light currently used to visualise the fatty build-up found in arteries (atherosclerotic plaques) they could selectively identify the rupture-prone deposits, which commonly lead to blood clots, heart attacks and strokes.
While some fatty deposits or plaques can remain stable for years, other high-risk cases develop complications, such as bleeding into the plaque, which leads to the formation of cracks and rupture of the fatty plaque. This can result in blockages in the blood vessels causing a heart attack or stroke. Current imaging techniques are able to identify some characteristics of high-risk plaques but none are generally accepted as reliable methods for selectively detecting the dangerous plaques.
“What we have done uses innovative, materials-based techniques to assist in the development of new diagnostic tools,” explains Dr Tara Schiller, WMG, University of Warwick.
“This could help us to detect the threat of an imminent heart attack and result in a decrease of the mortality rates,” Dr Schiller continues.
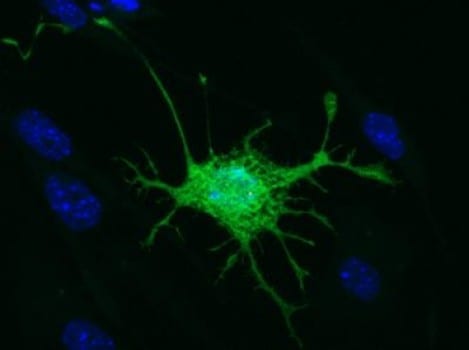
Dr Tara Schiller from the International Institute for Nanocomposites Manufacturing at WMG, along with colleagues from the Baker and Monash University, have discovered that increasing the wavelength of the infra-red (IR) radiation currently used to detect fatty deposit build-up in arteries to near-infrared (NIR) wavelengths allowed them to selectively identify plaques with internal bleeding, typically associated with high-risk deposits.
The products causing this fluorescence were identified using Raman spectroscopy. They are thought to be a mixture of heme products, formed during the degradation of red blood cells. These products were only observed in the unstable plaques with internal bleeding and not observed in the more stable fatty deposits. This can improve selectivity when looking for high-risk deposits in patients and could help doctors to identify the most at-risk patients.
“Despite the millions of dollars spent each year particularly on heart imaging, there still isn’t a reliable way of identifying these unstable plaques,” explains Dr Karlheinz Peter.
“We realised when we shine a light in the near-infrared wavelength range, that this light is reflected at a certain wavelength. So in a way we can use laser light to shine up the plaques that are unstable, and it’s very characteristic,” Dr Peter continues.
After further investigation with clinical trials this method of imaging technique could be used to assess unstable fatty arterial plaques and could be used to monitor the effectiveness of the drugs used to prevent heart attacks or strokes.
Learn more: Lasers used to detect risk of heart attack and stroke
The Latest on: Heart attack and stroke detection
[google_news title=”” keyword=”heart attack and stroke detection” num_posts=”10″ blurb_length=”0″ show_thumb=”left”]- Morning Heart Attack Symptoms: 7 Warning Signs That Shouldn't Be Ignoredon May 8, 2024 at 1:44 am
Here's how your body tells you about an impending heart attack. Read the article to know about the bodily symptoms of heart attack that can show up in the morning.
- New Data: 70% of Heart Attack and Stroke Patients Were Unaware This “Bad” Symptom Affected Themon May 7, 2024 at 5:09 am
A new American Heart Association survey found that heart attack and stroke survivors were unfamiliar with a key cholesterol clue. The post New Data: 70% of Heart Attack and Stroke Patients Were ...
- Heart Disease Newson May 5, 2024 at 5:00 pm
A Blood Test for Stroke Risk ... a smartphone to analyze heart movement and detect heart ... Unnecessary Use of Beta-Blockers After a Heart Attack? Apr. 8, 2024 — Half of all patients discharged ...
- High BP in childhood may raise heart attack, stroke risk by 4x, finds studyon May 3, 2024 at 9:36 pm
Untreated high blood pressure in children poses significant risks, including heart, kidney, and brain damage. Lifestyle modifications and early detect ...
- Being Angry for Just 8 Minutes Could Increase Risk of Heart Attack and Stroke, Study Sayson May 1, 2024 at 4:08 pm
A new study from the Journal of the American Heart Association reveals that those who suffer from anger management may have increased risk for heart attacks and strokes.
- 5 women’s health tips to prevent and detect strokes, according to cardiologistson April 25, 2024 at 2:30 am
One in five women between the ages of 55 and 75 will experience a stroke. Parag Shah, MD, a physical medicine specialist in Jacksonville, Florida, shares tips for women to reduce their risk.
- Is It a Stroke or a Heart Attack?on April 10, 2024 at 5:00 pm
Both stroke and heart attack symptoms occur suddenly. Though the two events have a few possible symptoms in common, their other symptoms differ. A common symptom of a stroke is a sudden and ...
- How Does Air Pollution Affect The Risk Of Heart Attack And Stroke? A Review By Doctorson March 28, 2024 at 11:00 am
Air pollution can increase the risk of heart attack and stroke in a number of ways. Air pollution can irritate the airways and lungs, making it difficult for the heart to pump blood. This can lead ...
- This Diet Can Lower Your Threat of Heart Attack and Stroke (Even If You're High Risk)on April 2, 2023 at 6:57 am
A meta-analysis of 40 clinical trials links the Mediterranean diet to a lowered risk of heart attack and stroke. The diet was the most effective at lowering risk of any eating plans studied.
- Heart Disease Detection Goes High Techon December 20, 2020 at 11:32 pm
From blood tests to advances in imaging, here are a few highlights in heart disease detection ... most likely to rupture and cause a heart attack or stroke. But in the future, blood tests may ...
via Google News and Bing News