Cells from patients’ blood could be developed as treatments for heart and circulatory diseases.
Scientists have shed light on a common bleeding disorder by growing and analysing stem cells from patients’ blood to discover the cause of the disease in individual patients.
The technique may enable doctors to prescribe more effective treatments according to the defects identified in patients’ cells.
In future, this approach could go much further: these same cells could be grown, manipulated, and applied as treatments for diseases of the heart, blood and circulation, including heart attacks and haemophilia.
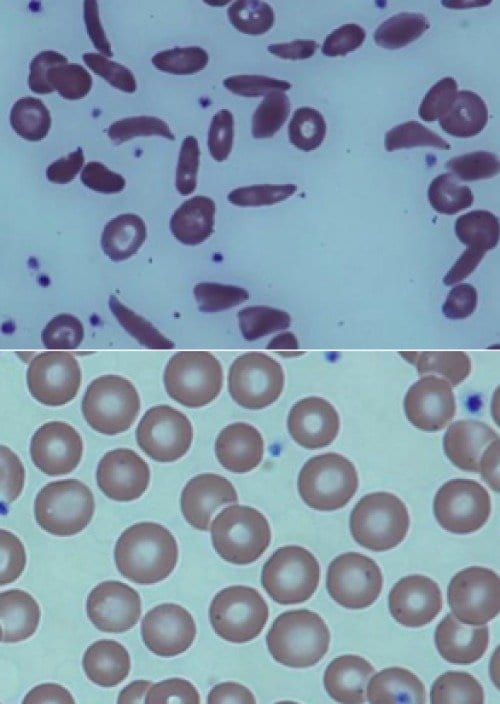
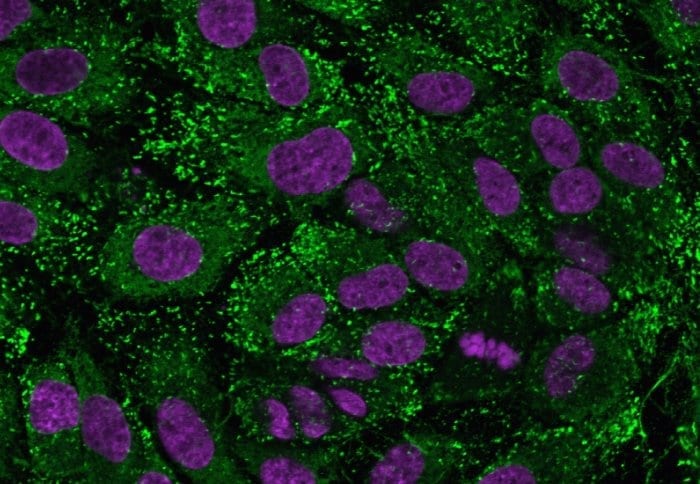
The study focused on von Willebrand disease (vWD), which is estimated to affect 1 in 100 people and can cause excessive, sometimes life-threatening bleeding. vWD is caused by a deficiency of von Willebrand factor (vWF), a blood component involved in making blood clot. vWF is produced by endothelial cells, which line the inside of every blood vessel in our body. Unfortunately, they are difficult to study because taking biopsies from patients is invasive and unpleasant.
A group led by Dr Anna Randi at the National Heart and Lung Institute,Imperial College London used a new approach to investigate the disease. Dr Richard Starke, a British Heart Foundation Intermediate Fellow and lead author of the study, took routine blood samples from eight patients with vWD, extracted stem cells called endothelial progenitor cells, and grew them in the lab to yield large numbers of endothelial cells.
By testing these cells, they were able to analyse each patient’s disease in unprecedented detail. In some patients, the scientists found new types of defect, which may enable them to recommend improved treatments. Professor Mike Laffan, a collaborator in the study and in charge of patients with VWD at Hammersmith Hospital in West London, is looking to apply these findings to reduce severe bleeding in these patients.
Dr Randi believes that endothelial progenitor cells could become an invaluable resource for testing new drugs for vWD and other diseases. “We will be able to test the effects of a range of compounds in the patients’ own cells, before giving the drugs to the patients themselves,” she said.
This approach could have impact far beyond vWD. Endothelial cells derived from blood could also be isolated and reinjected into someone recovering from a heart attack, to help them grow new blood vessels and repair the injured heart tissue. Dr Starke says this approach avoids the main problem with transplant therapies, in which the immune system tries to destroy the foreign material. “The patients would receive their own cells, so they wouldn’t face the problems of rejection,” he said.
Work is well underway towards achieving this goal, but blood-derived endothelial cells are only now being explored. “There are already many studies where patients have been injected with stem cells to see whether damage to the heart could be repaired, and there are some promising results,” says Dr Randi. “The door is open to such treatments, and our studies are a step towards identifying the right cells to use.”
The Latest Bing News on:
Stem cell therapy
- Celebrities Quietly Paying Huge Amounts for Anti-Aging Stem Cell Therapy That May Cause Gruesome Side Effectson April 27, 2024 at 6:31 am
Experts caution that there's limited evidence backing the benefits of these stem cell treatments, while pointing to plenty of risks.
- Cancer patient has ground-breaking new treatment at Colchester Hospitalon April 27, 2024 at 5:00 am
aiding in eliminating the cancerous cells. Jo Rosier, research team lead for haematology at Colchester Hospital, said: "This drug is an exciting step in the treatment options for people with bone ...
- I tried 60 minutes of hyperbaric oxygen therapy for the first time — here’s what happened to my bodyon April 26, 2024 at 10:30 pm
Hyperbaric oxygen therapy (HBOT) encourages the natural healing process by increasing oxygen uptake in a controlled and pressurized environment. This could be the recovery tool for you if you’re ...
- New prototype that regenerates stem cells may repair IPF scarringon April 26, 2024 at 10:42 am
Researchers developed NZ-97, an inhalable drug that stimulates the growth of stem cells in the lungs, potentially repairing scarring in IPF.
- Secret to eternal youth? John Cleese extols virtues of stem cell treatmenton April 26, 2024 at 9:12 am
Therapy has remarkable medical potential but experts say private clinics making far-reaching claims operate in regulatory grey zone ...
- Therapeutic potential of human umbilical cord-derived mesenchymal stem cells in Crohn’s diseaseon April 25, 2024 at 6:00 am
Whether human umbilical cord-derived mesenchymal stem cells (hUC-MSCs) could heal luminal ulcers in Crohn’s disease.
- John Cleese is spending thousands on stem cell therapy – is it really the secret to anti-ageing?on April 24, 2024 at 9:59 pm
The procedure in question is stem cell therapy, a treatment that the Monty Python star undergoes every 12 to 18 months. “These cells travel around the body and when they discover a place that needs ...
- John Cleese is spending thousands on stem cell therapy – is it really the secret to anti-ageing?on April 24, 2024 at 5:00 pm
Yet this isn’t a flash-in-the-pan craze for Cleese: he’s apparently been undergoing stem cell therapy for around two decades, and believes that “buying yourself a few extra years” makes ...
- New device improves stem cell generation and chance for accessible Alzheimer's cell therapyon April 24, 2024 at 12:11 pm
Researchers in Sweden say they have improved on a technique for converting regular skin cells into neural stem cells—an advance that they say helps close the gap for accessible personalized cell-based ...
- The murky, unregulated world of anti-ageing stem cell therapyon April 24, 2024 at 11:52 am
The latest taker is 84-year-old John Cleese, who revealed in an interview earlier this week that he pays £17,000 every 12 to 18 months on private stem cell therapy in the hope of buying “a few ...
The Latest Google Headlines on:
Stem cell therapy
[google_news title=”” keyword=”stem cell therapy” num_posts=”10″ blurb_length=”0″ show_thumb=”left”] [/vc_column_text]The Latest Bing News on:
Personalized medicine
- Personalized 'cocktails' of antibiotics, probiotics and prebiotics hold promise in treating IBS, pilot study findson April 26, 2024 at 3:10 pm
Personalized "cocktails" of antibiotics, probiotics and prebiotics hold great promise in the treatment of a common form of irritable bowel syndrome (IBS), according to research presented at the ESCMID ...
- 'Despite promise, personalized medicine for head and neck cancers facing hurdles'on April 26, 2024 at 3:45 am
Improved efficacy: By identifying specific mutations driving tumour growth, personalized medicine allows for targeted therapies that have a higher success rate compared to ‘one-size-fits-all’ ...
- Examining the impact of gene-based breeding on agriculture and medicineon April 25, 2024 at 10:22 am
A research team has demonstrated that gene-based breeding (GBB) offers a transformative approach to advancing plant and animal breeding, showing remarkable predictability, speed, and ...
- Calories, gut health and food as medicine — with AdventHealth’s Karen Corbin and a local culinary medicine specialist (podcast)on April 24, 2024 at 9:00 pm
In this episode of the Inspiring Wholeness podcast, AdventHealth’s Karen Corbin and Allison Harrell, sole practitioner and culinary medicine specialist, discuss calories, gut health and food as ...
- AI could predict whether cancer treatments will work, experts say: ‘Exciting time in medicine'on April 23, 2024 at 3:00 am
A chemotherapy alternative called immunotherapy is showing promise in treating cancer — and a new artificial intelligence tool could help ensure that patients have the best possible experience.
- 8 Clinical Trials That Will Shape Medicine in 2024on April 22, 2024 at 10:13 am
One of the exciting things about modern medicine is that it is making increasingly rapid advancements in a number of key areas. These advancements could have a major impact on the future of medicine.
- Progesterone Therapy in Demand for Personalized Medicine: Market to Reach US$4.8 Billion by 2034 | Future Market Insights, Inc.on April 22, 2024 at 3:30 am
After extensive research, the progesterone market suggests an upward trajectory from 2024 to 2034, inferring a healthy CAGR of 12.30%. With preliminary valuations of US$ 1.50 billion in 2024, the ...
- How AI can help cancer patients receive personalized and precise treatment fasteron April 16, 2024 at 1:35 pm
Providence and Microsoft are developing research prototype AI tools to sort through growing mountains of patient data.
- The Future of Breast Cancer Care: Blackwood on Personalized Approacheson April 15, 2024 at 8:01 am
In this episode of Targeted Talks, M. Michele Blackwood, MD, FACS, discusses the current landscape of breast cancer treatment and how personalized medicine with genomic testing is changing the field.
- Readers respond to OTC antidepressants, personalized medicine, restoring trust in public health, and moreon April 12, 2024 at 5:00 pm
This essay supports my assertion that the fiscal issues that might hinder the usefulness of personalized medicine need to be dealt with at the same time as we continue our progress towards large-scale ...
The Latest Google Headlines on:
Personalized medicine
[google_news title=”” keyword=”personalized medicine” num_posts=”10″ blurb_length=”0″ show_thumb=”left”]